Project Description
HATI – HIV Awal (Early) Testing and Treatment Indonesia
For decades, the global movements on HIV/AIDS have strived to achieve the 90-90-90 goals. What does it mean? First, people should have access to knowing their HIV status. Secondly, people diagnosed with HIV have all the access to receiving antiretroviral therapy. Lastly, their access to the therapy is sustained throughout their lifetime. In a way, we will have: 1) the 90% of all people living with HIV will know their HIV status; 2) 90% of all people with diagnosed HIV infection will receive sustained antiretroviral therapy, 3) 90% of all people receiving antiretroviral therapy will have viral suppression.
In Indonesia, aiming for 90-90-90 seems ambitious, yet it is achievable. Many HIV studies are on their way to assist the government on this mission, including HATI Study. It stands for Study on HIV Awal (Early) Test and Treat Indonesia (HATI Study). This implementation research prospectively evaluates strategies to improve the cascade of HIV care in key populations.
Funding



Collaborators



Duration
2015-2020
Principal Investigator
Yanri Wijayanti Subronto
These key populations are men sex with men, transgender, female sex worker and people injected with drugs. For five years of study (2015-2020), HATI has conducted five interventions in elaborating which strategies are the most efficient in boosting the HIV cascade of care.
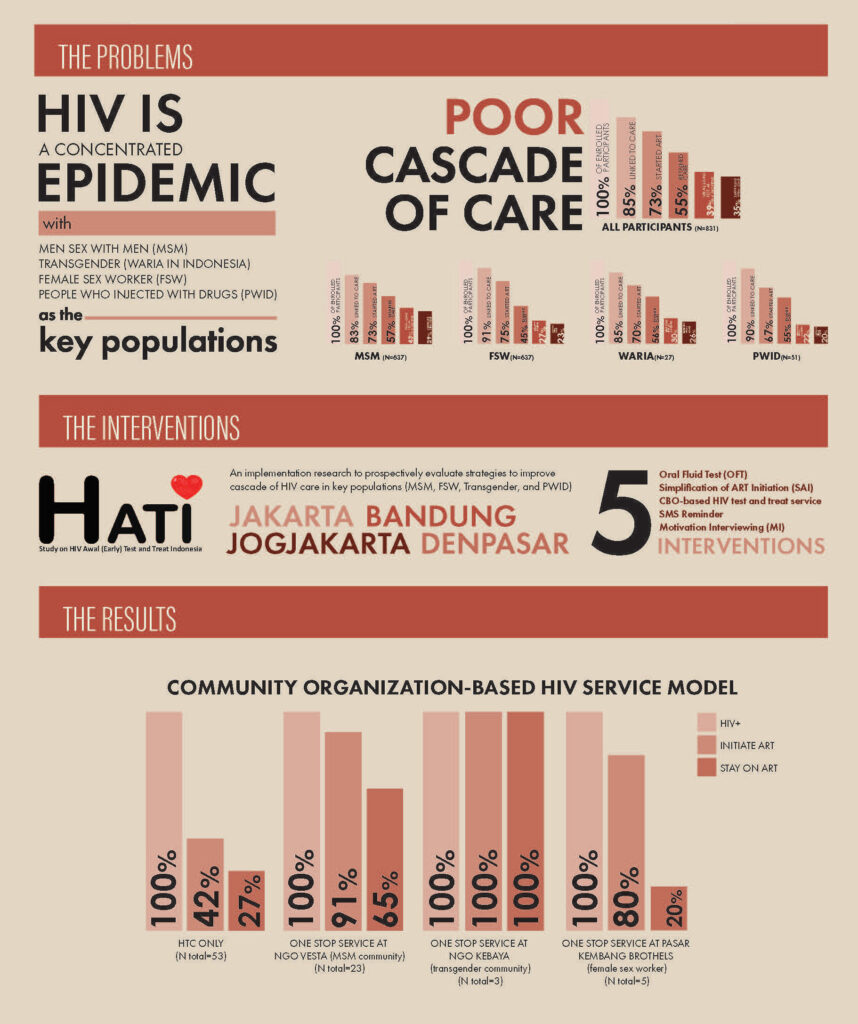
The most highlighted intervention from the HATI study is the community-based HIV service model. This approach provides HIV tests and treatment in non-health facility settings, including among the marginal communities.
The results of this model were so promising. It significantly increased the number of both
new and re-testing uptake of ART initiation and adherence, especially for the communities of men sex with men and transgender people.
Published Works
Januraga, P., Reekie, J., Mulyani, T., Lestari, B., Iskandar, S., Wisaksana, R., Kusmayanti, N., Subronto, Y., Widyanthini, D., Wirawan, D., Wongso, L., Sudewo, A., Sukmaningrum, E., Nisa, T., Prabowo, B., Law, M., Cooper, D. and Kaldor, J., 2018. The cascade of HIV care among key populations in Indonesia: a prospective cohort study. The Lancet HIV, 5(10), pp.e560-e568.
Lazuardi, E., Newman, C., Anintya, I., Rowe, E., Wirawan, D., Wisaksana, R., Subronto, Y., Kusmayanti, N., Iskandar, S., Kaldor, J. and Bell, S., 2019. Increasing HIV treatment access, uptake and use among men who have sex with men in urban Indonesia: evidence from a qualitative study in three cities. Health Policy and Planning: The Journal on Health Policy and System Research, vol. 35(1), pp 16-25
Lazuardi, E., Newman, C., Tasya, I., Rowe, E., Wirawan, D., Wisaksana, R., Subronto, Y., Kaldor, J., Kusmayanti, N., Iskandar, S. and Bell, S., 2019. Understanding the Social Influences on Engaging Key Populations With HIV Prevention: A Qualitative Study With Men Who Have Sex With Men in Three Indonesian Cities. AIDS Education and Prevention, 31(3), pp.206-223.
Mitchell, E., Lazuardi, E., Rowe, E., Anintya, I., Wirawan, D., Wisaksana, R., Subronto, Y., Prameswari, H., Kaldor, J. and Bell, S., 2019. Barriers and Enablers to HIV Care Among Waria (Transgender Women) in Indonesia: A Qualitative Study. AIDS Education and Prevention, 31(6), pp.538-552.
Widyanthini, D., Januraga, P., Wisaksana, R., Subronto, Y., Sukmaningrum, E., Kusmayanti, N., Dewi, H., Law, M., Kaldor, J. and Wirawan, D., 2021. HIV self-testing for men who have sex with men: an implementation trial in Indonesia. AIDS Care, pp.1-8.
The Project Team